Blogs
- Home
- Blogs
- Educational
- IVF Timeline Guide from Start to Finish

IVF Timeline Guide from Start to Finish
May 27, 2025Molly Chu Chen - Labryo Fertility
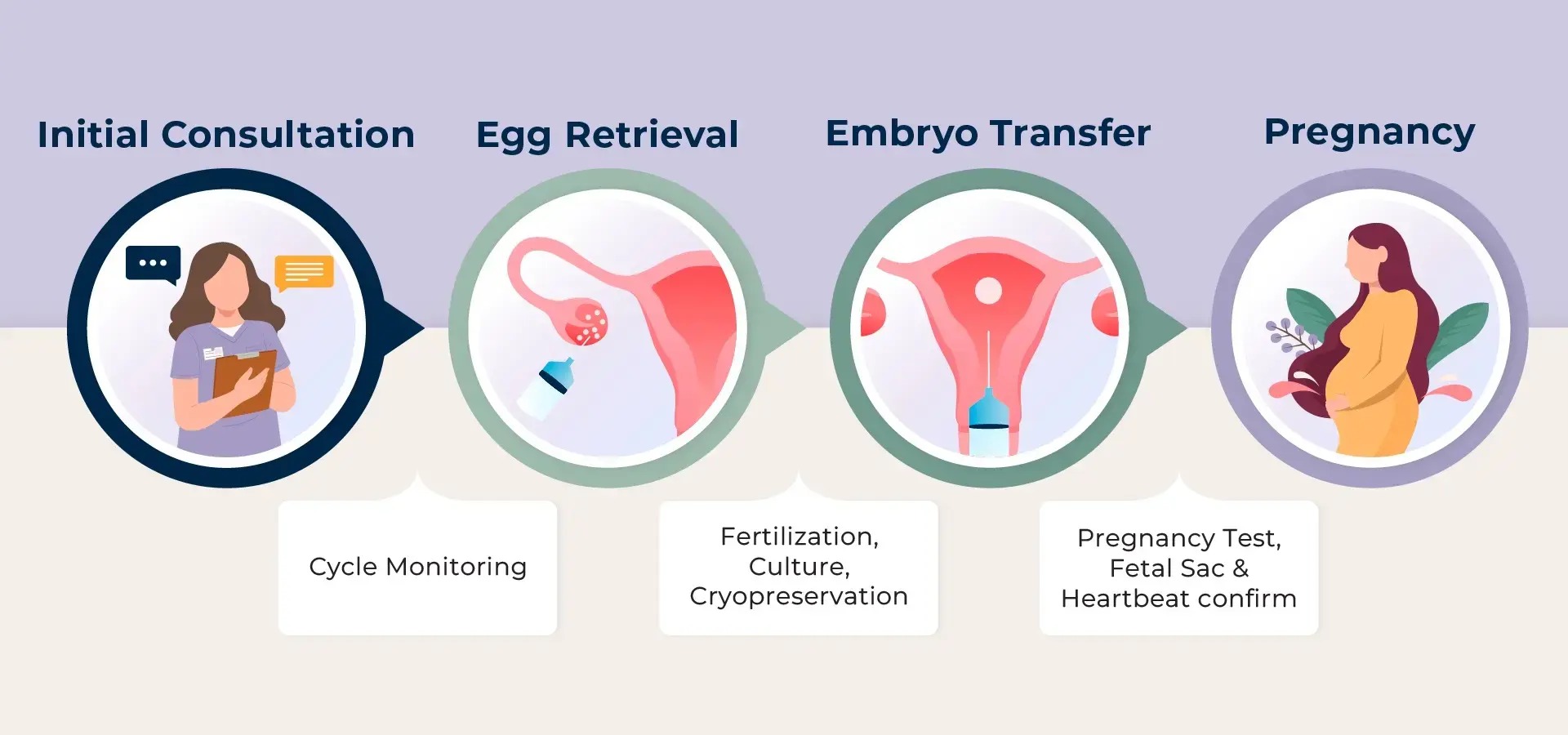
EducationalBeginning the in-vitro fertilization (IVF) journey is both a hopeful and deeply personal decision—one that involves emotional strength, physical commitment, and thoughtful preparation. Understanding each phase of the IVF timeline can help ease uncertainty and empower you to make informed decisions. At Labryo Fertility Center, we’re here to guide and support you every step of the way, so we’ll outline how long the process will take in this guide, preparing you for what’s ahead.
Overview: How Long Does the Entire IVF Process Take?
While every IVF journey is unique, a typical cycle—from the start of consultation to frozen embryo transfer—usually takes about 8 weeks. The exact timeline can vary based on individual health, age, fertility diagnosis, medical history, potential genetic diseases, and the treatment plan recommended.
The Standard IVF Timeline: A Step-by-Step Breakdown
For your reference, here’s a step-by-step breakdown of a standard IVF cycle, including how long each phase typically takes from start to finish.
Step 1. Initial Consultation and Fertility Assessment: 2–4 Weeks
The first step in the IVF process is scheduling an initial consultation with a fertility specialist. This meeting is a critical starting point, where your physician will review your medical history in detail, discuss any previous fertility treatments, and your goals (how many babies you would like to have) to determine whether IVF is the right path forward. It’s also a time to ask questions, share concerns, and begin shaping a care plan that’s tailored to your unique needs.
Following the consultation, a comprehensive series of fertility assessments is conducted. For female patients, this often includes bloodwork to check hormone levels (like AMH and FSH), thyroid function, and screening for infectious diseases. A pelvic transvaginal ultrasound and saline infusion sonogram (SIS) are also performed to assess the uterus and ovaries, while ovarian reserve testing helps estimate the number and quality of remaining eggs. Genetic carrier screening may also be recommended, depending on your family history or ethnicity, and also if you are planning to use a donor.
On the other hand, male partners typically undergo a semen analysis and may also be asked to complete infectious disease testing and genetic screening.
This phase also includes a financial consultation to review IVF costs, insurance coverage, and available treatment packages. Consent forms are signed during this period, and results from all tests are gathered to inform the next steps.
Altogether, the consultation and testing phase can take two to four weeks, depending on individual circumstances.
Step 2. Ovarian Stimulation: 10–14 Days
Once your treatment plan is finalized, the next phase is ovarian stimulation, typically lasting 10 to 14 days starting from the 2nd or 3rd day of your menstrual cycle. During this time, you’ll begin daily hormone injections (e.g. Gonadotropins such as Follistim or Gonal-F) or take oral medications (e.g. Clomiphene citrate like Clomid) to encourage your ovaries to produce multiple eggs instead of the single egg usually released in a natural cycle.
The goal is to increase the number of mature eggs available for fertilization, which can improve your chances of a successful IVF outcome. The specific type of medication you use will depend on your physical situation and the doctor’s recommendations.
Your body’s response to the medications will be closely monitored throughout this period. You’ll come in every 3 to 5 days for regular ultrasounds to measure the growth and number of developing follicles, as well as blood tests to track hormone levels, particularly estrogen.
Based on these screening results, your physician may adjust your medication dosage to ensure optimal stimulation while minimizing the risk of complications such as ovarian hyperstimulation syndrome (OHSS).

Source: Freepik
Step 3. Trigger Injection: 1–2 Days
When your follicles have reached the right size, a trigger shot is administered—typically containing human chorionic gonadotropin (hCG) or a gonadotropin-releasing hormone (GnRH) agonist—to prompt the final maturation of eggs and prepare them for retrieval about 36 hours later.
Step 4. Egg Retrieval: 1 Day
Egg retrieval is a short outpatient procedure performed without anesthesia or under light sedation, typically taking 10 to 30 minutes. Guided by a transvaginal ultrasound, your physician uses a thin needle to gently aspirate the fluid from each mature follicle in the ovaries. This fluid, which contains the eggs, is immediately passed to the IVF laboratory, where embryologists inspect and prepare the eggs for fertilization.
Following the procedure, you'll rest in a recovery area for about an hour and then be discharged once your care team confirms there aren’t any issues. The care team will also provide personalized post-procedure instructions, including signs to watch for and when to begin the next steps in your treatment.
Nevertheless, most patients may experience mild cramping or bloating, which usually resolves within a day. It's generally recommended to rest for the remainder of the day but many patients typically feel well enough to resume normal activities the next day. If necessary, over-the-counter pain medicine is enough to provide relief, just consult your care team to make sure you get something suitable.
Step 5. Sperm Collection and Fertilization: 1 Day (Same Day as Egg Retrieval)
On the same day as egg retrieval, the sperm sample—either freshly collected or previously frozen—is processed to isolate the healthiest, most motile sperm. The selected sperm are then used to fertilize the mature eggs using conventional IVF or ICSI.
In conventional IVF, eggs and sperm are placed together in a petri dish, allowing fertilization to occur naturally as the sperm swim to penetrate the egg. Alternatively, when male factor infertility is present or if fertilization rates have been low in previous cycles, the physician may recommend using intracytoplasmic sperm injection (ICSI) instead. In ICSI, a single sperm is carefully injected directly into each mature egg using a fine needle, increasing the chances of successful fertilization.

Source: Freepik
Step 6. Embryo Development: 5–7 Days
After fertilization, embryos are carefully cultured in a controlled laboratory for 3 to 7 days. During this time, they are monitored for cell division and growth rate, as our embryologists assess their overall quality based on established grading criteria.
At Labryo Fertility Center, we use advanced technology like the EmbryoScope—a time-lapse imaging system that allows continuous observation without disturbing the embryos. This technology helps our embryologists identify the healthiest embryos with the best developmental potential while keeping them in a consistent environment for safety.
By days 5 to 7, the embryos ideally reach the blastocyst phase, which is the optimal stage for embryo biopsy, embryo transfer, or freezing (cryopreservation).
Step 7. Genetic Testing: 2–6 Weeks (Optional)
Preimplantation Genetic Testing (PGT) is an optional step that allows embryos to be screened for genetic abnormalities before transfer. A few cells are carefully biopsied from each embryo and tested to assess chromosomal health or identify inherited genetic conditions. This testing can help reduce the risk of miscarriage and increase the chances of a healthy pregnancy. It can also be used to know the sex beforehand.
This step may extend the overall IVF timeline by 2 to 6 weeks and the embryos are frozen while awaiting results. Moreover, PGT may incur additional costs, so the doctor or medical coordinator will make sure it aligns with your budget before proceeding.
It is also important to note that there are different kinds of PGT. If you are interested in learning more about what each type of PGT tests for, as well as the process and benefits, you can check out our full article: What is PGT-A & Who Should Consider It?

Source: Freepik
Step 8. Uterine Preparation: 2-4 Weeks
Before embryo transfer, patients—especially those undergoing a frozen embryo transfer (FET)—may need hormone therapy to prepare the uterus for implantation. The therapy starts after egg retrieval and includes 2 to 3 weeks of estrogen to thicken the uterine lining, followed by 1 week of progesterone to support embryo implantation and early pregnancy, creating the optimal environment for the embryo to attach and grow. Additionally, hormone support often continues through the first trimester to promote a healthy and stable pregnancy.
Step 9. Embryo Transfer: 1 Day
Embryo transfer is a quick and typically painless procedure in which one or more embryos are carefully placed into the uterus using a thin, flexible catheter. The entire process usually takes 10–15 minutes and doesn’t require anesthesia.
This step can involve either a fresh transfer, performed a few days after egg retrieval and fertilization, or a frozen embryo transfer (FET), where a previously frozen embryo is thawed and transferred at an optimal time. FET is usually preferred as it offers flexibility in timing and allows the procedure to be performed as a separate cycle, where the focus can be on optimal conditions for the uterus. It also enables patients to have additional time for preimplantation genetic testing (PGT).
Step 10. Pregnancy Screening: 2 Weeks and Beyond
The period following embryo transfer—often called the "two-week wait (TWW)”—can be one of the most emotionally intense parts of the IVF journey. During this time, it’s natural to feel hopeful, anxious, or even uncertain.
Around 10 to 14 days after transfer, a blood test is performed to measure levels of hCG, a hormone that signals early pregnancy. While some may notice mild pregnancy-like symptoms such as bloating, fatigue, or breast tenderness, these signs can also result from hormone medications. It’s important not to read too much into symptoms alone and always consult with your physician before making any decisions.
A confirmed positive result marks a major milestone, but your fertility clinic will continue to monitor your hCG levels and schedule follow-up ultrasounds to ensure everything is progressing well. If the test is negative, your care team will guide you through the next steps and support your options moving forward.
Factors Influencing the IVF Timeline
Source: Freepik
It's important to understand that while we've outlined a typical IVF timeline, several variables can influence the duration of the process. Recognizing these factors allows for a clearer understanding of your journey.
- Age: A woman's age, particularly her ovarian reserve and egg quality, is a significant factor affecting the IVF timeline and success rates. Older patients may require different medication protocols or experience fewer eggs retrieved, so it may influence the number of embryo transfer attempts and extend the timeline.
- Underlying Fertility Issues: Conditions such as polycystic ovary syndrome (PCOS), endometriosis, uterine fibroids, or male factor infertility can necessitate specific treatment approaches and may impact the timeline. For instance, managing PCOS might involve a longer stimulation phase to avoid over-stimulation.
- Response to Medications: Individuals respond differently to ovarian stimulation medications. Some may require adjustments in dosage or a longer stimulation period to achieve optimal follicle development, thus affecting the overall timeline.
- Use of Donor Eggs or Sperm: Incorporating donated sperm or eggs into the IVF process often involves additional steps, such as donor selection, screening, and coordination, which can extend the overall timeline.
- Egg Retrieval and Embryo Transfer Outcome: The number of mature eggs retrieved and whether embryos implanted successfully can affect the timeline as patients and the fertility team decide on a plan to improve outcomes in the next steps.
- Choosing Double Ovarian Stimulation (DuoStim): In some cases, patients may opt for two egg retrievals within the same cycle if they have a sufficient follicle count. This approach will be performed during both the follicular and luteal phases, helping maximize egg yield in a shorter timeframe. Nevertheless, it’s not suitable for everyone and depends on the doctor’s recommendation.
- Fertility Goal: The number of children the intended parents hope to have affects how many eggs they should retrieve and how many retrieval cycles they would need. For example, if a patient wishes to have 2 children, it may be advisable to aim for at least 15 eggs total. Then, if she retrieves 2-3 eggs per cycle, it could take 3-4 retrievals to get all the eggs, extending the process accordingly.
Because every patient is unique, clinics like Labryo Fertility Center create personalized treatment plans to address these variables and optimize each individual’s chances of IVF success while improving their time to pregnancy.
When to Try Again After a Failed IVF Cycle?
After a Failed Egg Retrieval
If your egg retrieval cycle did not result in viable embryos, it’s natural to feel disappointed. Typically, your menstrual period will begin 1–2 weeks after the procedure, giving your ovaries a chance to recover. In most cases, you can begin your next stimulation cycle with your following period.
However, your doctor may recommend additional rest before proceeding, depending on how your body responded to the medications in previous attempts. Your physician will also conduct a thorough review of the previous cycle to identify any potential adjustments to the protocol for the next attempt.
After a Failed Embryo Transfer
When an embryo transfer doesn’t result in pregnancy, you can usually try again relatively soon. A menstrual period typically begins about a week after a negative pregnancy test. If there are no medical concerns, your next embryo transfer may be scheduled within that same cycle.
With that said, it's crucial to have a detailed consultation with your fertility specialist to discuss the potential reasons for the transfer failure and to determine the optimal modifications to the process for your next attempt. Plus, emotional readiness is just as important. If you need more time, your care team can help tailor a treatment plan that suits your physical and emotional well-being. Moreover, the fertility specialist may also offer some additional therapy or alternative options to help you on this journey to parenthood.
Start Your IVF Journey with Labryo Fertility Center
At Labryo Fertility Center, we understand that the IVF process can feel overwhelming—which is why we’re here to guide you every step of the way. One of the tools we provide to help patients stay organized is a personalized IVF calendar. This calendar tracks your appointments, medication schedule, lab work, and procedures, ensuring you always know what’s coming next. It’s designed to streamline your experience and reduce the stress that can come with fertility treatments.
Our expert team will also work closely with each patient to build a customized treatment plan tailored to your medical needs, lifestyle, and goals. From your initial consultation to egg retrieval, embryo transfer, and beyond, Labryo Fertility Center is committed to providing compassionate, high-quality care at every stage of the journey.
If you are ready to take the next step, feel free to fill out our contact form today and let Labryo Fertility Center help you take the first step toward growing your family.

