Blogs
- Home
- Blogs
- Educational
- What are the Success Rates of IVF?
What are the Success Rates of IVF?
December 27, 2024Molly Chu Chen - Labryo Fertility
EducationalIn Vitro Fertilization (IVF) is one of the most widely used assisted reproductive technologies (ART) for individuals and couples facing infertility. It involves fertilizing an egg with sperm in a laboratory dish. Once fertilized, the embryo is transferred to the uterus, where it can implant and develop.


According to the Centers for Disease Control and Prevention (CDC) clinic data summary, the average IVF success rate in the U.S. is 48.12%, meaning nearly half of all embryo transfers result in a live birth. While this figure is encouraging, actual outcomes can vary significantly depending on personal circumstances.
In this article, we’ll break down IVF success rates in more detail, explore the key factors that influence them, and share practical tips on how to improve your chances throughout the treatment journey.
1. IVF Success Rates on Average
A successful IVF cycle is typically defined as an embryo transfer that results in a live birth. The births can either be singleton births, where only one baby is born, or multiple gestational births, where twins, triplets, etc., are delivered, often due to the transfer of multiple embryos.
As mentioned, the embryo transfer success rate for IVF is 48.12%, based on 108,601 embryo transfers conducted in a year within the U.S. region. Among these, 41.4% result in singleton births, as most intended parents may aim to reduce the risks associated with multiple gestation pregnancies.
However, it’s important to note that the percentage above is merely an average. The success rate of an IVF cycle depends on each individual, as it can vary significantly due to factors like the patient’s age, the quality of the eggs or embryos, whether or not PGT testing was performed, the expertise and knowledge of the medical team, and the specific treatment protocols used. Hence, modern fertility clinics will take a personalized medical approach for each patient to optimize the outcomes.
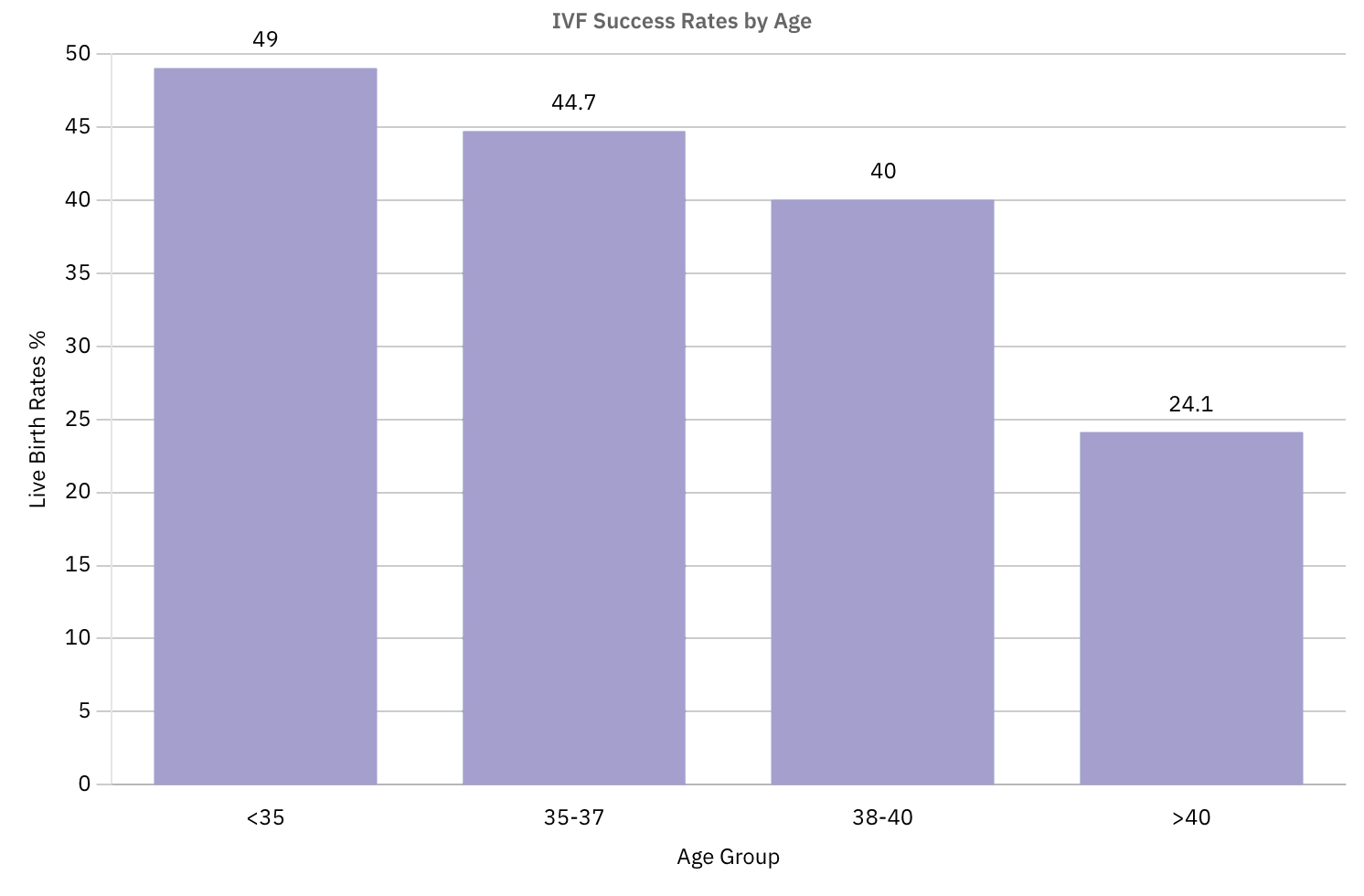
2. IVF Success Rates by Age When Using Patient’s Own Eggs
In this section, we will outline the in vitro fertilization success rates by age. This information is particularly relevant for patients who plan to use their own eggs, as the egg quantity and quality naturally decline with age.
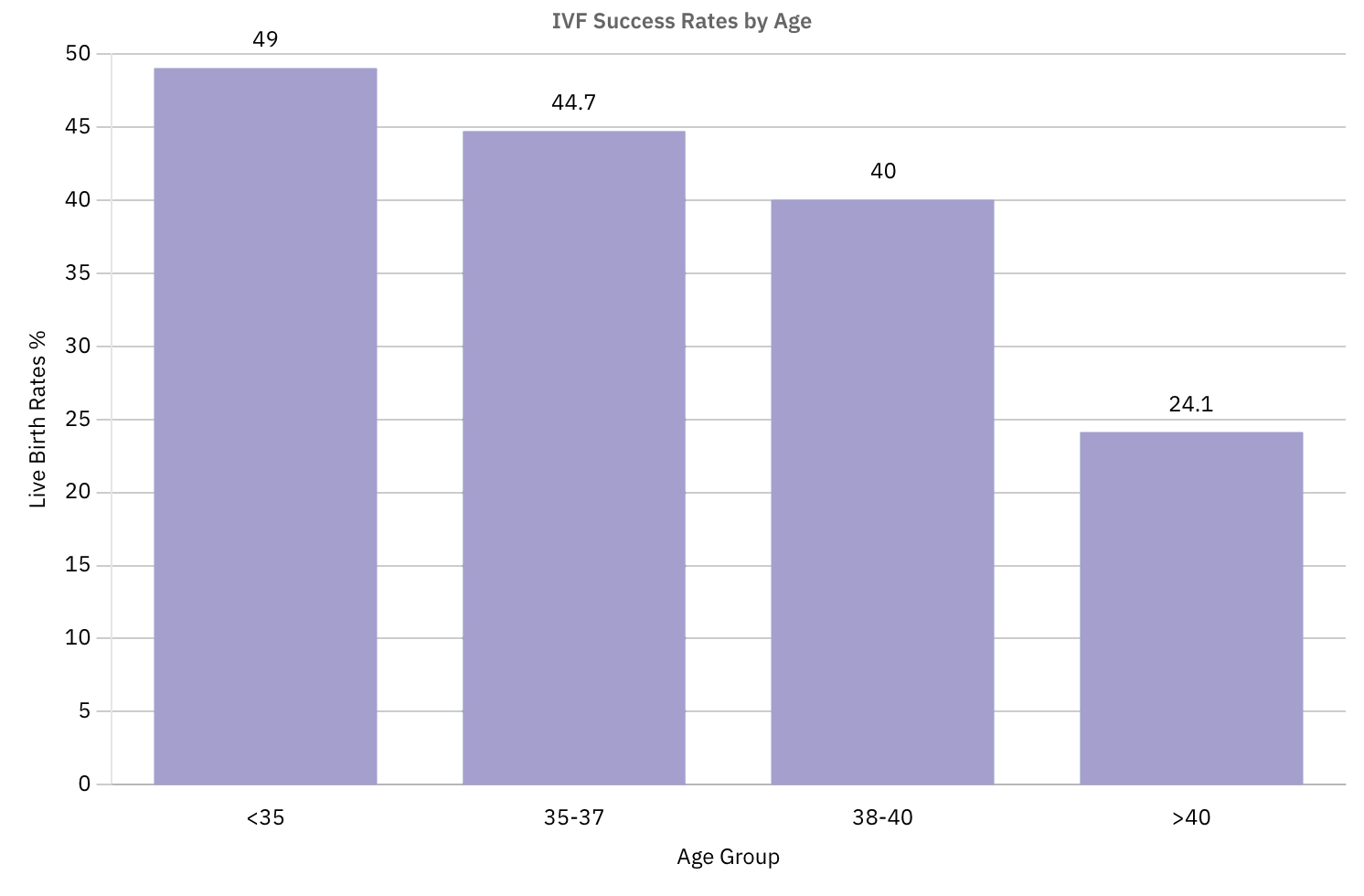
The following table summarizes the IVF success rates according to different age groups:
| Age Group | Under 35 | 35 to 37 | 38 to 40 | Over 40 |
| Total Embryo Transfers |
54,052 |
26,846 |
18,578 |
9,125 |
| Live Birth Rates |
49.0% |
44.7% |
40.0% |
24.1% |
| Singleton Birth Rates |
45.4% |
42.0% |
37.8% |
23.0% |
Source: CDC Database
The IVF success rates for women under 35 are the highest with 49% of the embryo transfers resulting in live births. Consequently, the women aged 35 to 37 experience a moderate decline to around 44%, while those aged 38 have approximately a 40% chance of success. Furthermore, the IVF success rates for women over 40 will drop more sharply to around 24%, as seen in the bar chart below:
3. IVF Success Rates When Using Donor Eggs
Some patients may choose to use donor eggs to increase egg transfer success rates, as donor eggs often come from younger individuals meticulously pre-screened by health professionals to improve the chances of implantation and live birth from IVF.
This option is particularly beneficial in cases of premature ovarian failure, early menopause, genetic disorders, or any other reasons that may cause the patient to have a lack of healthy eggs.
If the patient does choose to use a donor egg, they will also have to decide whether to use fresh embryo transfer or frozen embryo transfer for the IVF process. Fresh embryo transfers involve fertilization and immediate embryo transfer following egg retrieval, while frozen embryo transfers allow embryos to be cryopreserved through advanced vitrification techniques for later use.
Here’s a comparison of the success rates using donor eggs through fresh and frozen embryo transfers:
| Embryo Type | Fresh | Frozen |
| Total Transfers |
1,113 |
17,775 |
| Live Birth Rates |
53.5% |
46.3% |
| Singleton Birth Rates |
49.3% |
43.5% |
Source: CDC Database
Both methods provide excellent success rates. The choice often depends on the patient’s circumstances. Some patients may opt for frozen embryo transfer as it offers more flexibility for their schedules and personal circumstances while allowing for PGT testing. If more time is needed until the patient’s uterine lining and hormonal environment are fit for implantation, the embryos will be kept safely through vitrification in a lab, allowing the patients more time to prepare for the transfer cycle after egg retrieval.
4. The Success Rates of IVF vs IUI
Intrauterine Insemination (IUI), also known as artificial insemination, is another common fertility treatment option, where sperm is directly placed into the uterus. While the procedure is less complicated and more cost-effective, IUI generally offers lower success rates than IVF.
A 2022 study published in the Archives of Gynecology and Obstetrics found that the success rates of IUI are approximately 10.9% to 19.4%. In contrast, IVF success rates per cycle can range from 25% to over 50%, depending on individual patient factors. This makes IVF a more effective option for many, especially those facing more complex fertility challenges.
5. Factors that Influence IVF Success Rates
Next, we will explore the key factors affecting IVF success rates to help patients make informed decisions as they pursue this journey to parenthood.
5.1. Maternal Age
As we’ve mentioned earlier, a woman’s age and IVF success rates are closely related, especially when they are using their own eggs for the treatment. A woman’s ovarian reserve will gradually diminish as they age and this decline usually becomes more noticeable after age 35, accelerating further when reaching beyond the age of 40.
A low ovarian reserve results in a lower quantity and quality of eggs, which means there are lower chances of producing viable embryos for successful implantation. Even if the embryos implant successfully, poor egg quality can still lead to embryos with chromosomal abnormalities which could potentially increase the risk of miscarriage or birth defects.
5.2. Individual Infertility Conditions
Specific infertility issues in both men and women can significantly influence IVF success rates. For women, common factors include uterine lining issues, such as thin endometrial lining or uterine fibroids, which can hinder embryo implantation. Ovulatory disorders like polycystic ovary syndrome (PCOS) and endometriosis can also reduce success rates as these medical conditions usually affect egg quality.
For men, low sperm count, poor sperm motility, or abnormal morphology can impact fertilization success. In some cases, male factor infertility may require additional interventions like intracytoplasmic sperm injection (ICSI) to improve outcomes.
In such cases, patients should consult with their fertility specialists to evaluate their health condition and determine the most effective approach for IVF treatments.
5.3. Number of IVF Cycles
Patients may require multiple IVF cycles to achieve a successful pregnancy depending on factors like individual health conditions, egg quality, and embryo viability.
In some cases, multiple retrieval cycles are necessary to obtain eggs and create a healthy, viable embryo. Similarly, multiple transfer cycles may be required to achieve implantation and sustain a pregnancy.
On average, most patients undergo two to three embryo transfer cycles before achieving success, though some may need more. A helpful way to evaluate each cycle is through the “Three E’s” approach. The E’s stands for Endometrium, Embryo, and Embryo Transfer. This framework looks at the uterine lining (its thickness and appearance), the embryo's grade (based on cell development and structure), and the ease of the transfer procedure itself. By assessing these three factors, fertility specialists can make more informed adjustments for future cycles to improve outcomes.
Nevertheless, IVF is rarely a one-and-done treatment, so it’s important to stay patient and work closely with your doctor to optimize each step along the way.
5.4. Pregnancy History
Studies in the journal Fertility and Sterility have shown that individuals who have successfully conceived with their current partner in the past are more likely to achieve conception through IVF. This history suggests that the uterine environment and sperm compatibility may be favorable.
On the other hand, a history of repeated miscarriage or pregnancy complications could imply lower IVF success rates, as this may indicate uterine abnormalities, hormonal imbalances, or genetic issues. This is why fertility specialists will carefully assess reproductive history to tailor treatment strategies and improve the chances of a successful pregnancy. Some patients also consider gestational surrogacy as a solution to minimize these risks.
5.5. Individual Lifestyle
Research published in Reproductive BioMedicine has shown that lifestyle factors can significantly impact IVF success rates. Smoking, in particular, can negatively affect egg and sperm quality, as well as reduce blood flow to the uterus, hindering implantation.
Additionally, both underweight and overweight individuals may experience reduced IVF success rates due to hormone imbalance and reduced egg quality.
5.6. Fertility Clinic Expertise and Protocols
Choosing a clinic with a proven track record, modern protocols, and an experienced medical team can significantly improve the likelihood of a successful IVF cycle. Experienced clinics offer comprehensive health evaluations to assess intended parents for a detailed understanding of underlying conditions. This personalized approach enables specialists to recommend customized treatment plans, with optimal hormone medication dosage, egg retrieval timing, and embryo transfer procedures to improve outcomes.
It is also important to choose a clinic with skilled IVF laboratory capabilities. Advanced IVF labs with experienced embryologists and state-of-the-art technology ensure precise embryo handling, monitoring, and culturing. In turn, this provides a better condition to improve embryo quality for IVF treatments.
6. How to Improve the Chances of Success with IVF
While there's no guaranteed way to improve IVF success rates, adopting a healthy lifestyle and following your doctor's advice can significantly enhance your chances. Here are some tips to consider:
- Maintain a Healthy Weight: Research by the Canadian Medical Association has shown that a healthy weight is crucial for optimal IVF outcomes. Aim for a BMI within a healthy range to maintain better hormone levels and egg quality.
- Follow a Balanced Diet: Try eating plenty of fruits, vegetables, whole grains, and lean proteins to make sure the body has enough nutrients to maintain a healthy condition. Studies in the Nutrients Journal even suggest that a Mediterranean diet can be helpful during ART treatments. You can consult your fertility specialist to find a diet program that works best for you during the treatment.
- Exercise Regularly: Incorporate regular exercise into your routine. According to the Journal of Physical Activity and Health, regular physical activity improves blood circulation and hormone regulation, which is essential for reproductive health. However, if you have underlying conditions like PCOS or endometriosis, it’s more important to consult your physician regarding what kind of exercises you should do. Different exercise regimes should be implemented for each individual depending on their condition.
- Avoid Alcohol and Tobacco: No alcohol or tobacco should be used during the IVF process. Based on studies in the journal Reproductive BioMedicine, both these substances can significantly affect egg and sperm quality, reducing IVF success rates.
- Manage Stress: Practicing relaxation techniques such as meditation, yoga, or deep breathing exercises can help reduce stress. This, in turn, can support hormonal balance and improve fertility, as shown in research by Fertility and Sterility.
- Choose a Reputable Clinic: When selecting a fertility clinic, consider factors like the experience of the medical team, availability of in-house IVF lab facilities, and patient-centered care. Moreover, look for board-certified reproductive endocrinologists, transparent success rates, and up-to-date IVF technologies. Patient testimonials and personalized consultation options can also help you gauge whether the clinic aligns with your medical and emotional needs throughout the IVF journey.
- Follow Doctor's Instructions: Patients always follow the doctor’s advice during treatment, especially for medication regimens and appointment schedules. The treatment plan is usually based on the patient’s individual circumstances. So, it is important to adhere to them for a smooth IVF cycle.
7. Start Your IVF Journey at Labryo Fertility Center
Embark on your journey to parenthood with Labryo Fertility Center, a leading fertility clinic dedicated to providing high-quality, personalized fertility treatments.
With a team of experienced specialists, we offer comprehensive services to support you from the initial consultation to IVF procedures, and every step will be carefully tailored to meet your unique circumstances.
At Labryo Fertility Center, our state-of-the-art IVF lab is equipped with the latest technology to ensure optimal embryo development. Plus, our skilled embryologists will meticulously monitor every stage of the process, helping you achieve high-quality outcomes during treatment.
Moreover, Labryo Fertility Center offers transparent and affordable pricing options, with packages that cover essential IVF costs for egg retrieval, sperm preparation, embryo culture, and embryo transfer, without any hidden costs. We’ve also partnered with Future Family to provide personalized loans, making IVF treatments more accessible to a wider range of patients.
Want to learn more? Visit our IVF page for more details or contact us today to schedule a consultation. We will make sure you receive the best possible care throughout the entire process.
Insights on IVF Success Rates from Our Experts
Labryo Fertility Center is dedicated to empower patients on their fertility journey with the facts. As such, this article is brought to you by Molly Chu-Chen and Dr. Jeremy A. King for reliable information regarding IVF outcomes.
Molly Chu-Chen, M.S., M.H.A., TS (ABB) - Chief Embryologist & Founder
At the heart of Labryo Fertility Center’s IVF success is Molly Chu-Chen’s meticulous approach to embryo development. With more than 20 years of embryology experience, Molly’s leadership ensures the facility maintains consistent, high-performing protocols in egg handling, fertilization, and embryo transfer. Her certification from the American Board of Bioanalysis and hands-on management of each case further drive the outcomes that matter most to patients—healthy pregnancies and live births that fulfill their dreams of creating a family.

At the heart of Labryo Fertility Center’s IVF success is Molly Chu-Chen’s meticulous approach to embryo development. With more than 20 years of embryology experience, Molly’s leadership ensures the facility maintains consistent, high-performing protocols in egg handling, fertilization, and embryo transfer. Her certification from the American Board of Bioanalysis and hands-on management of each case further drive the outcomes that matter most to patients—healthy pregnancies and live births that fulfill their dreams of creating a family.
Dr. Jeremy A. King, M.D. - Director of IVF

Dr. Jeremy King has a track record of elevating IVF success rates through strategic, patient-specific care. As Labryo Fertility Center’s IVF Director, his extensive research background in hormone function and infertility—honed at Johns Hopkins—translates into precise stimulation protocols and embryo transfer timing. His previous leadership in military IVF clinics has also earned national recognition, and he continues to apply his knowledge to maximize success for every patient.
